Maine health care workers are subject to a near-daily barrage of physical and verbal assaults from patients or their family members, nearly a dozen doctors, nurses and administrators from area hospitals said in interviews with the Sun Journal.
And while the “ripple effects of the pandemic” have contributed to a rise in violence against health care workers over the past 2½ years, the issue predates COVID-19 and often goes underdiscussed, the workers said.
It is also why the workers expressed a sense of relief and gratitude that the issue has received renewed attention in the form of a recently formed legislative task force to study the criminal process by which perpetrators can be held responsible for their actions.
The task force — a bipartisan group of lawmakers and members of the medical, law enforcement and judicial fields in Maine — will submit its report this fall.
Violence can happen in any health care setting, but it is of particular concern for those who work in hospital emergency departments, intensive care units and psychiatric units.
“I think the important thing to remember about (violence) is that it’s an escalation of something,” said Dr. John Alexander, chief medical officer for Central Maine Healthcare in Lewiston.
“People don’t just walk in the door and begin, you know, verbally attacking others — or certainly physically attacking others. They come in under a great amount of duress and stress and strain, some of them with preexisting mental health illness — some of them perhaps not diagnosed — and others under just incredible, you know, incredible burden of what they’re going through,” he said.
The circumstances created by the pandemic, including longer wait times in emergency department waiting rooms, are adding to the stress.
Incidents at Central Maine Medical Center in Lewiston where security had to intervene increased by about a third from 2019-21, according to data provided by the hospital.
According to data from St. Mary’s Regional Medical Center’s workplace violence task force, from 2019-20, there were four times as many assaults on staff members at the Lewiston hospital, and five times as many from 2019-21.
Emergency department staff are in a particularly difficult position, Alexander and others said, because they are at the first point at which an individual enters a hospital. The individual may be experiencing a mental health crisis or be in a lot of pain or discomfort. That, coupled with how — especially now — emergency departments are dealing with long wait times, a patient or a companion may get agitated and act aggressively.
“It’s something that I have to think about on a daily basis,” said Courtney Ryder, the Emergency Department nursing director at Franklin Memorial Hospital in Farmington.
“I need to be aware of who’s in the department, what the potential threats there might be,” she said.
Christina Booth, the Emergency Department nurse director at Stephens Memorial Hospital in Norway, said staff must prepare for violent incidents before a patient even steps into the unit.
She said at SMH, the workplace violence committee has evaluated the hospital’s facilities to make them safer. That includes, for example, bolting picture frames to the walls so that they cannot be removed and used as a weapon, and installing panic buttons and badge access-only doors in the Emergency Department.
Other workers described subtle tactics they learn, such as making sure that a patient is never between them and an exit in case they need to make a quick escape.
But there is only so much that staff can do to prepare for violence.

Nurse Kristi Dugan demonstrates her medical staff training Thursday to keep herself between a potentially violent patient and a door at St. Mary’s Regional Medical Center in Lewiston. Andree Kehn/Sun Journal
WHAT’S OUT OF HOSPITAL WORKERS’ CONTROL
Hospital staff take anyone who comes through their doors as mandated by both their oath to the communities they serve and by federal law, SMH President Andrea Patstone said.
The opioid crisis and, more recently, the flood of illicitly manufactured methamphetamine, a type of stimulant, into Maine has “definitely created some strain,” said Dr. Jim Gallea, the Emergency Department medical director at SMH.
That strain sometimes comes from individuals who are seeking medications that the providers do not feel comfortable prescribing, he said. Other times it comes from individuals who are going through drug or alcohol withdrawal or who are highly intoxicated.
Heather Nadeau, Emergency Department nurse leader at St. Mary’s, said there’s been a notable uptick in individuals coming into the Emergency Department who have taken meth, often mixing it with alcohol. “The drugs that they’re taking are making them more violent.”
St. Mary’s chief medical officer for behavioral health, Dr. Michael Kelley, said these patients can be “acutely psychotic and violent. And they don’t respond as well to our traditional medications that calm people down either.”
These patients may need to be physically restrained or require sedatives to calm them down. In those cases, patients need to be monitored in an intensive care unit, said one former ICU nurse, who asked not to be named because of professional concerns.
The nurse said it is as if those patients, especially those on meth, “have the strength of 10 men.”
“They are strong, and they are violent, and all they want to do is to clear the path and get out,” she said.
The nurse, who has worked in hospitals in Maine and other states, said most of the acts of violence directed at her were perpetrated by an individual in withdrawal or who was intoxicated.
She described one incident where she was kicked in the face by a young man high on bath salts. Another time, while the nurse was 8 1/2 months pregnant, a “withdrawing alcoholic” kicked her in the stomach.

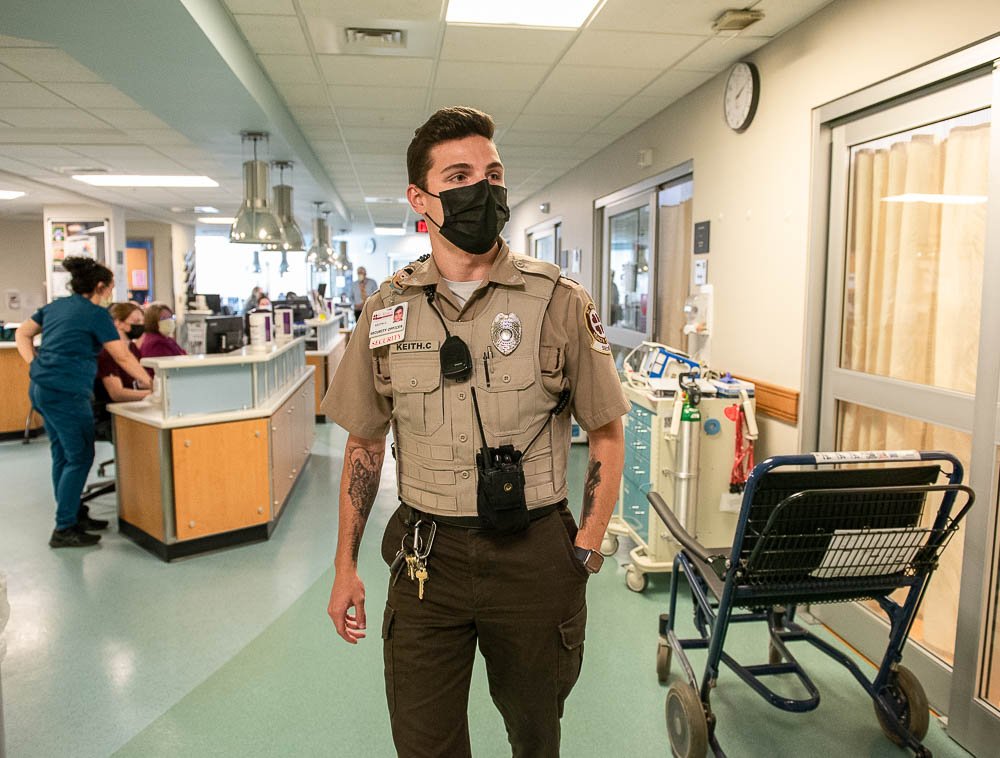
Keith C. does rounds Thursday at St. Mary’s Regional Medical Center in Lewiston. He is a hospital-trained security officer ready in case a “Code Gray” is called, which is triggered by violence or potentially dangerous behavior from patients or visitors. Andree Kehn/Sun Journal
Sometimes these individuals are brought in by police. Maine lacks an infrastructure equipped to provide medical and psychiatric care to people who are violent or are criminal offenders, and this has made hospitals, and in particular emergency departments, a catchall solution for bridging the gap between the behavioral health and judicial systems, several of the workers told the Sun Journal.
“We’re seeing a lot more patients coming in from the community that you would typically see go to jail (that) are now coming to a hospital setting for stabilization and management,” Nadeau said.
Kelley said in other states, these individuals would be handled through a forensic psychiatry system, a subset of psychiatry where clinicians are trained to handle the complexities at the intersection of mental health care and law enforcement.
Hospitals or other health care settings with forensic psychiatry units are also more secure than a typical hospital or are a medical unit within a jail or prison, Kelley said.
Instead, he said that in his experience in Maine, when police arrest someone who needs psychiatric attention, they “almost exclusively” bring them to the Emergency Department first.
“And then they’re going to tell us you need to get them stable enough to go to jail, which, unfortunately, leads to assaults because we’re not currently trained and there’s no way to get somebody into the forensic system (in Maine) where they’re trained to deal with mental health patients that have criminal behaviors,” he said.
VIOLENCE ALSO PROMPTED BY PAIN, FEAR
Not all patients who are experiencing a mental health crisis or are intoxicated are violent, however. And not all individuals who get aggressive fall into either of those categories.
“There’s plenty of medically induced reasons that could cause the patient to be violent” or verbally aggressive, Nadeau said.
When a patient is in pain, uncomfortable or confused, they can get irritable.
“We understand that, you know, we want to be supportive to our patients, but they can lash out,” she said.
There are often older patients who have dementia or another cognitive disorder who come into the hospital for an unrelated medical reason and become extremely confused and agitated.
Booth, from Stephens Memorial, said when she was a new nurse, the first patient “I ever got punched by was an 85-year-old gentleman who was scared for his life. Like, he did not understand that he had just had a heart attack and he was getting a cardiac procedure.”
Gallea, the SMH doctor, said the issue of verbal aggression shouldn’t get lost in the conversation about violence.
“It’s probably the more frequent and more common occurrence and the thing that ultimately is very insidious in terms of the impact and the consequences that it has on our staff,” he said.
Dr. David Gammons, an attending physician at Franklin Memorial’s Emergency Department, said he “cannot tell you the number of times” that he has been verbally assaulted or threatened with physical violence.
“It is something that comes up almost every time I come into work, at least in my mind,” he said. “And it does wear on you, especially when people verbally accost you. It makes an already difficult job that much harder (and) I think most people in health care would probably agree with that.”
About half of the workers interviewed for this story said they’re more concerned about threats and assaults from family members of patients rather than patients.
Gallea, for example, described a situation from his residency that he said has affected him more than any other incident.
He said a family member of a patient was upset about something involving the patient and began sending Gallea threatening emails. Then, the man showed up at the emergency department where Gallea was working at the time, managed to slip through the doors that went from the waiting room and onto the patient floor, and started asking for him.
A colleague noticed the man acting in an odd manner and tried to redirect him by telling him that Gallea wasn’t there, and alerted security.
“When in fact, I was actually like in the next room seeing a patient,” he said. According to Gallea, the man told security, “I’m looking for Dr. Gallea but it’s OK, I know where he lives.”
At that point, Gallea said he was ushered out another door. The hospital put him and his wife up in a hotel for a week as a precaution.
“That was pretty scary,” he said. “You know, going to my house that evening after that all occurred with sort of a security presence to pack my bags was pretty eerie.”
THE ‘RIPPLE EFFECTS OF THE PANDEMIC’
“COVID is very peripheral to this,” Kelley, from St. Mary’s, said.
But the ways in which COVID has impacted all aspects of the health care system have certainly made things worse. Many workers have left the profession for a multitude of reasons, but especially because of burnout, which has exacerbated preexisting staffing shortages.
“The supports outside of the hospital have diminished drastically,” Kelley said. There are fewer group homes, fewer nursing homes, fewer case managers, fewer community-based treatment programs, he said.
“And so, the patients that were held together by those supports are falling apart and then they show up in the emergency room.”

Steve Costello, vice president for business development and communication, demonstrates Thursday the triage procedure used by staff for patients entering the Behavioral Emergency Department at St. Mary’s Regional Medical Center in Lewiston. Keith C., a hospital security officer, holds a paper bag in which a patient or visitor deposits all metal objects, including cellphones, wallets, watches and jewelry, all of which are returned when the person leaves the facility. Andree Kehn/Sun Journal
Fewer outside resources have also created a backlog of patients in the hospitals. With fewer beds at nursing homes and group homes available, patients are waiting longer to be discharged, which means fewer patients from the emergency department can get admitted.
The overflow of patients has been especially apparent in the Behavioral Emergency Department, Kelley said. In 2019, the average length of stay from the time a patient entered the Emergency Department to the time they left, either because they were admitted or discharged, was eight hours. Right now, the average is about 48 hours.
St. Mary’s is the only hospital in the area that has both an inpatient adult and pediatric behavioral health unit and oversees psychiatry services at Community Clinical Services. The Emergency Department, including the waiting rooms, are divided into medical and behavioral units.
CMMC offers inpatient psychiatric consultations for emergencies but most patients are transferred to a different facility, like St. Mary’s, if they need long-term inpatient care.
“Whereas three years ago, we might have (had) eight to 14 patients a day in the emergency room, now we’re starting off the day with 12 people that have been there overnight and then adding another 20 patients during the day,” to the behavioral Emergency Department, which sometimes flows over into the medical Emergency Department, Kelley said.
“So then you get crowded emergency rooms,” filled with patients there for psychiatric and medical emergencies. “And they’re all irritated,” he said.
Staff on workers’ compensation leave for injuries sustained during an assault doubled from 2019-21, according to St. Mary’s.
“It’s very clear that (there are) many more assaults and the assaults are much worse than they were,” Kelley said.
Alexander, from CMH, agreed with Kelley’s assessment that “it’s not COVID itself, but it is the circumstances of the pandemic.”
“Mostly, we’ve been talking about just COVID itself and the infection and the risk of bringing it home and the strain of the pandemic,” like staff shortages.
“All of those things have been true,” Alexander said. “And yet this is, this has always been, in the background and we have seen an increase in the number of acts of aggression toward health care workers.”
Next week: The complex reasons why, health care workers say, there is a lack of recourse for them after violent incidents, and how they hope the legislative task force and other initiatives will help.
Send questions/comments to the editors.






Success. Please wait for the page to reload. If the page does not reload within 5 seconds, please refresh the page.
Enter your email and password to access comments.
Hi, to comment on stories you must . This profile is in addition to your subscription and website login.
Already have a commenting profile? .
Invalid username/password.
Please check your email to confirm and complete your registration.
Only subscribers are eligible to post comments. Please subscribe or login first for digital access. Here’s why.
Use the form below to reset your password. When you've submitted your account email, we will send an email with a reset code.